

The Torch Magazine, The Journal and Magazine of the
International Association of Torch Clubs
For 93 Years
A Peer-Reviewed
Quality Controlled
Publication
ISSN Print 0040-9440
ISSN Online 2330-9261
Volume 92, Issue 1
|
Medicine
and War:
Military Medical Advances in the Context of World War I by
Gerald Stulc
War is a
ravening beast, consuming like a
conflagration whatever and whomever
best serves its sustenance. World War
I, the Great War, was different in one
significant way: it exploited the most
significant advances in science and
technology as no other war before, or
since. This was so both regarding
weaponry (the tank, the airplane,
poison gas) and regarding the healing
of the wounded. The provision of
medicine in war is a paradox, the
story of compassion by the few in the
presence of neither by the many.
The 19th century saw exponential progress in biological sciences, knowledge essential for the advancement of the medical and surgical arts. New ways of killing made WWI a mire of industrial battlefields (Preston), but ten major medical-surgical advances were also appropriated and refined by that war. Several involved and drove surgical specialties, others utilized new discoveries in physiology and chemistry, and one dealt with the psychology of men at war. All were essential in precluding an otherwise far greater death toll, and established military medical care pertinent to this day. The introduction of immunizations and disinfecting techniques for surgery and wound treatment were the first significant breakthroughs exploited in WWI. In the latter part of the 19th century, specific bacteria and viruses, "germs," were recognized as the causes of infectious diseases. Ignaz Semmelweis and Joseph Lister used the "germ theory" to establish antiseptic principles in surgery, markedly decreasing postoperative infections and deaths. WWI was the first conflict wherein surgeons regularly operated and treated wounds antiseptically, including Lister's disinfectant, carbolic acid. (1) During the war, French surgeon Alexis Carrel, a Nobel prize recipient, worked with English chemist Henry Dakin to develop a potent antiseptic solution for wounds: Carrel-Dakin's solution, sodium hypochlorite, a weak bleach still employed medically today (Dunne 284). Immunizations came to be used widely by both Allied and Central powers—the German and Austro-Hungarian Empires. Typhoid vaccine was first administered to British troops in the Second Boer War (1899-1902). Soon, active investigations were underway for vaccinations against many bacterial and viral infections, such as tetanus. British military surgeons serving in the Boer War had dealt with wounding sustained in hot dry soil that was relatively sterile, but the fertile soils of France and Belgium, composting centuries of manure, allowed the Clostridium bacteria that caused tetanus and gangrene to flourish in fields and wounds alike. By WWI, antitoxins were available against tetanus, "lockjaw," but in the first months of the war tetanus cases were rampant among wounded troops. Initiating routine administration of tetanus antitoxin to the wounded dramatically decreased the incidence of tetanus on both sides (Scotland and Hays). The second major advance concerned the treatment of physiological shock. Physiological shock was associated with severe wounding, and recognized since at least the dawning of the Age of Gunpowder. Shock from massive trauma (injury) caused pallor and coolness of the skin, decreased blood pressure, urine output and mental status, and increased heart rate—often progressing to death. The French coined the term choc for this constellation of signs in the 18th century, onomatopoeia for the sound of a musket ball striking flesh. At first, wound shock was erroneously thought to stem from poisoned musket balls. By WWI, competing scientific theories existed regarding the origin of shock, including direct damage to the brain from explosives (Scotland and Hayes 102-03). However, observations clearly related the level of shock, and its prognosis, to the degree of blood loss; restoring blood volume with salt water or blood reversed the downward spiral of shock in many of the wounded. (2) Fortunately, in 1904, Karl Landsteiner and Jan Janský had independently discovered the human blood groups, allowing for transfusions from matched donors to recipients. Blood transfusion techniques had been developed at Harvard, Johns Hopkins, and Queen's Belfast University hospitals in the years leading up to the war. During the war, blood transfusions for massive trauma-shock saved countless lives, though initially the British favored intravenous administration of saline or acacia gum solutions. The first blood transfusions were direct—attaching an artery in the donor's wrist to an arm vein in the wounded recipient. Obviously, this involved time and surgical expertise, impractical when a field hospital was inundated with hundreds of wounded in a single afternoon. Indirect transfusions speedily evolved. Blood could be collected in syringes coated with paraffin to preventing clotting, then injected into the blood into the patient. (3) In October 1915, Canadian surgeon Lawrence Robertson was the first to use this method to resuscitate a soldier wounded by multiple shrapnel, and consequently persuaded the Royal Army Medical Corps to adopt transfusions (Pelis). Based on the work of others, American surgeon Richard Lewisohn formulated a safe concentration of sodium citrate-dextrose to prevent blood from clotting, enabling the storage of blood. The American surgeon Oswald Robertson was the first to stock a blood bank in anticipation of the Battle of Cambria, November 1917, using ammunition cases for ice chests (Hess and Schmidt). Whole-blood transfusions became standard treatment for physiological (hemorrhagic) shock after the war. (4) Many historians consider the transfusion and banking of blood as the principal medical contribution of WWI. *
*
*
The
introduction of anesthesia and
antisepsis in the last decades of the
19th century permitted the development
of modern surgery. For the first time,
surgeons could enter the inner sancta
of the human body—the brain, chest,
and abdomen. In previous wars,
soldiers with serious head and "gut"
gunshot wounds were laid within the
shade of trees, given morphea, and
allowed a peaceful death. In WWI, men
receiving such injuries were pulled
from the muck of No Man's Land and
taken to surgery, with a better than
even chance of survival.
In WWI, 70% of injuries involved the extremities due to the randomness of shell bursts and shrapnel, 17% involved the head and neck, 4% the chest, <2% the abdomen, and 7% "other" ("Weapons Effects" 2). Salvage of life and limb, though, depended on rapid recovery and triage of the wounded, especially as medical advances permitted treating what had once been considered hopeless cases. Timely medical attention was appreciated a century earlier by Dominique Jean Larrey, Napoleon's Surgeon General, who designed the first ambulances "to afford speedy assistance to the wounded" (Larrey). In WWI, the French revalidated the concept with statistics describing the "The Golden Hour" (Santy). Their data inarguably showed trauma survival predicated upon prompt transfer in the first hours of wounding to proximate medical facilities. A delay in treatment past four hours resulted in rapidly increasing mortality. Emergent life-saving techniques were applied in the field—clearing airways of blood and debris, compressing exsanguinating wounds, and bandaging sucking chest wounds. Notably, tourniquets were condemned because of variable expertise in their use; delays in reaching a medical facility without intermittent tourniquet release often led to a gangrenous limb. The English, under Sir Arthur Sloggett, instituted the most efficient, organized system of medical transfers and accessibility. Initial medical care was delivered directly behind the front lines, the Regimental Aid Post, manned by 32 litter bearers and a Regimental Medical Officer. (5) Care consisted of dressings, fracture splints, shock treatment with warmed blankets and hot water bottles, and morphine. From there, motorized and horse-drawn ambulances carried the lightly wounded to the tent section of the Advanced Dressing Station, undergoing treatment before returned to the fighting. The seriously wounded were triaged to a formal dressing station for emergency hemorrhage control or amputation, hopeless cases given comfort. Survivors from the dressing station were driven to Central Clearing Stations (CCS) miles behind the lines. There, individual CCS's specialized in types of trauma (i.e., head, abdomen), and performed definitive surgery. Serious cases were stabilized and sent by train or ship to large base (stationary) or general hospitals for further treatment and recovery, or discharge. Significantly, the first recorded air transport of a wounded soldier occurred in 1917 in the Sinai Peninsula during a raid on Bir el Hassana. A British officer of the Imperial Camel Corps who had been shot in the ankle was flown from battlefield, south of El Arish, to hospital by a B.E.2c (Bleriot Experimental) two-seater biplane. The flight took 45 minutes for a journey that would have taken 3 days by land (Dolev). Head injuries—what the Allies called "head cases"—were frequent in WWI because of high explosive shells timed to burst above entrenched soldiers. Consequently, steel helmets were reintroduced in 1915, first by the French, as limited protection against showers of hot steel. The management of penetrating head wounds was contingent on recent advances in neurology, and drew on innovations in technique that predated the war, with neurosurgery pioneered by Sir William Macewen, Victor Horsley, and Swiss surgeon Theodor Kocher. Macewen and Horsley served with the British Expeditionary Force (BEF), practicing an art thought impossible only a generation earlier, and training a new generation of surgeons in the emerging specialty of neurosurgery. A student of Kocher's, Harvey Cushing, pioneered neurosurgery in America. Harvard University sent him to France in 1915 as head of an expeditionary medical hospital, then again in 1917 after the United States entered the war. One of his innovations was an electromagnet that, combined with x-ray localization, would extract steel shrapnel from brain wounds (Fig. 1). Figure
1
Sketch of Cushing’s electromagnet for extraction of shrapnel from the brain. Drawing by Dr. Harvey Cushing, from his memoir, From A Surgeon’s Journal: 1915-1918. Little, Brown, and Company: Boston, 1936, p. 177. 
In Cushing's memoir of his war
experiences, he wrote, "In the early
afternoon a large batch of wounded
were unexpectedly brought in—mostly
heads—men who had been lying out for
four days in craters in the rain,
without food. It is amazing what the
human animal can endure. Some of them
had maggots in their wounds. Then a
long operation on a sergeant with a
thing [shrapnel] in his brain and
ventricle [. . .] the magnet again
useful" (Cushing 177). Brain abscesses
and blood collections were drained,
bone fragments of fractured skulls
elevated and removed from brain
tissue—lessons proving invaluable in
subsequent periods of war and peace.
Anesthesia was essential for surgery on head, chest, and abdominal wounds. For neurosurgery, local Novocain was the safest anesthetic. For all other wounds, nitrous oxide was the inhaled anesthetic of choice, since most anesthetics exacerbated shock, and ether increased the incidence of bronchopneumonia. The delicate balance of anesthesia delivery thus necessitated a new specialty, that of anesthesiology. In contrast to head and abdominal injuries, penetrating chest wounds were potentially survivable if the heart or major vessels were uninjured. Pierre Duval, administrator of the French Army of Flanders, strongly advocated for early operation on chest injuries. By 1917, the American Expeditionary Force established criteria for thoracic surgery: open (sucking) chest wounds; large foreign bodies, i.e., shrapnel or clothing; massive lung hemorrhage; significant rib or sternum injuries; major injury to the diaphragm; and fluid or pus collections (empyema) within the chest cavity. The major limitation to chest surgery was collapse of the uninjured lung when air at atmospheric pressure entered the opened chest cavity—a problem not resolved until after the war. (6) Like surgery of the brain and chest, abdominal surgery had evolved in the civilian sector during the last decades of the 19th century, but abdominal operations were prohibited in war, as surgical interventions historically had proven futile. Abdominal injuries by their nature are acute, often life-threatening, especially in war; most abdominal injuries resulted in death on the battlefield. Those who survived were belatedly transported to forward hospitals, their condition deteriorated to an extent where surgery was useless: "A stoic fellow contemplates his eventration [disembowelment] without a gesture; under his shirt, a fluctuation, sticky, liquid, alive and warm, stomach, intestines... A bandage is placed on top, and he's carried off" (Delaporte). Military surgeons at the advent of WWI, therefore, advocated watchful waiting, "expectant treatment," of perforating abdominal injuries, although carrying an 80% mortality. This pessimism was refuted by Lithuanian princess and surgeon, Dr. Vera Gedroits—one of the first women Professors of Surgery. (7) In the Russo-Japanese War, as head of Red Cross hospital trains, she promoted abdominal surgery within three hours of wounding (Bennett). The success of her approach was adopted by the Russian medical establishment, but ignored by the West—likely, cases of gender and cultural bias. In 1915, though, Owen Richards, Royal Army Medical Corps, reported nine cases of immediate surgery for penetrating abdominal wounds. Though seven died, two with multiple small bowel perforations survived, though such injuries had heretofore been considered untreatable. Other military surgeons were inspired to attempt similar results, gaining the attention Sir Arthur Bowlby, Surgeon General, BEF. In June 1915, he issued a directive that all abdominal wounds receive expedited transport and surgery. By the end of the war, the mortality from abdominal wounds was virtually halved, establishing precedence for treatment of these injuries (Scotland and Hays 191-92). Most war injuries, as noted, involved the extremities, but scant medical research was spent toward the treatment of such wounds. This changed thanks to an eccentric chain smoker who characteristically wore a buttoned-up black coat, a naval cap, and a patch over one eye: Dr. Hugh Owen Thomas, founder of English orthopedics. The first in his family to earn a medical degree, he came from a long line of Welsh bonesetters, a family pedigree essential in honing his skills and intuition to pioneer the specialty of orthopedics, at that time a practice traditionally relegated to tradesmen. Among his many innovations treating bone disease and injury was the Thomas traction splint. (Figure 2). Figure
2
Thomas splint applied to litter patient, Broussey, France, April 20, 1918 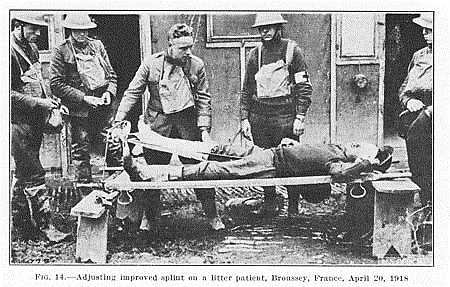
Apart from skull fractures, the
highest fatality rates for fractures
during WWI involved the femur
(thighbone)—approximating 80%. Femoral
fractures result in significant blood
loss. Bullets and shrapnel uniformly
cause open fractures and potentially
lethal infections. Thomas devised an
easily-applied traction splint which
kept the broken ends of bone stable
for transport to CCS's and surgical
debridement (Fig. 2). His nephew, Sir
Robert Jones, War Director of Medical
Orthopedics, introduced his uncle's
splint for femoral fractures, reducing
the mortality rate to 8% by the
Armistice. As a corollary, the great
number of men surviving serious
fractures and amputations necessitated
the new field of intensive
rehabilitation medicine and therapy.
*
*
*
Of all injuries,
the most tragically mutilating
involved the face, which the French
called gueules cassées,
"broken faces." High explosives burned
and shattered; petroleum fuel from
recently-invented internal combustion
engines ignited. Mixed with this lot
was a new horror, the flame-thrower.
Modern surgery and antisepsis salvaged
many injured soldiers and sailors, but
could not rebuild faces. Two
treatments were spearheaded by Harvard
dentist Varaztad Kazanjian: wiring of
shattered jaws and creating cosmetic
facial masks to replace missing
anatomy (Deranian).
Actual facial reconstruction, "plastic surgery," was initiated by New Zealand surgeon Harold Gillies, who almost singlehandedly developed plastic reconstructive surgery in WWI. Gillies had studied the reconstruction of faces disfigured by cancer surgery, subsequently inventing novel techniques and surgical instruments. (8) An early patient was a sailor badly burned on the ship Wasp during a naval engagement, who required numerous surgeries (Fig. 3).
Figure 3
Walter Yeo of the Warsprite, and facial burns sustained at the Battle of Jutland, 1916. Staged reconstructive surgery by Harold Gillies. 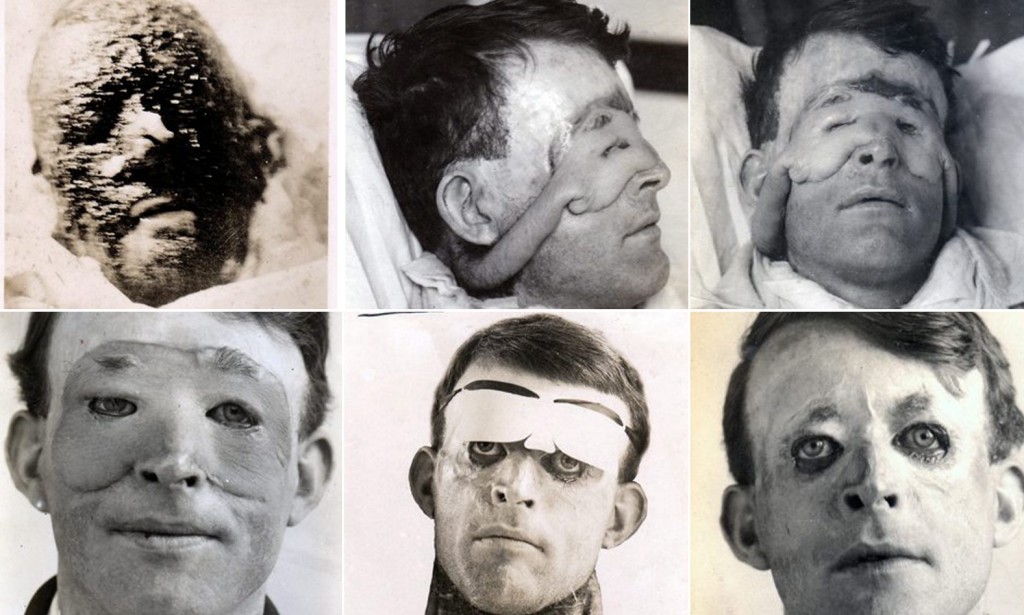
Gillies soon established a dedicated
hospital for plastic surgery at
Sidcup, England. The team he formed
there laid the foundations of plastic
surgery. It included Ivan Magill, who,
finding that the wire-gauze anesthetic
masks would not fit over injured
faces, precluding surgical access,
devised a tube for insertion down the
throat to administer anesthesia, the
forerunner of the endotracheal tube
used routinely by today's
anesthesiologists. Thousands of men
destined for lives of solitude and
despair were able to return to
society, thanks to Gillies. (9)
*
*
*
Theories of
physiological shock invoked disruption
of the central nervous system from
high explosives. When emotional
manifestations of prolonged combat
resulted in bizarre symptoms and
behavior in some soldiers, the natural
explanation was repetitive exposure to
explosive concussions. Physicians
designated it, "commotion of the
nervous system," or more commonly,
"shell shock," what is now termed Post
Traumatic Syndrome (PTS). Accordingly,
various medical and electrical
therapies were tried to restore proper
nerve conduction. Though unsuccessful,
these methods recognized a
neuro-biochemical basis for PTS.
Unfortunately, as psychiatry gained
devotees, shell shock became
considered a psychological aberrancy,
or a "lack of moral fibre"—attitudes
persisting to this day among certain
quarters of military and civilian
society. Recent studies estimate 20%
of soldiers in WWI, as in present
conflicts, experienced shell shock
(Winter). Medicine is returning to a
biological model of PTS, one that
recognizes physical neurological
damage and physiological stress as
major factors.
The last, and most incongruous, medical advance of WWI was the result of the gas warfare initiated in 1915. The threat from poison gas was more psychological than pragmatic, but sustained experimentation nevertheless led to the development of mustard gas. Though banned after the war, mustard gas continued to be studied by the United States Army. Exposure to mustard gas was found to markedly lower the body's white blood cells (Krumhaar). As a result, mustard compounds became the first cancer chemotherapy agents, used in the treatment of leukemias—the unregulated production of white blood cells.
*
*
*
The overall
impression might be that WWI
promulgated a variety of significant
advances in medicine and surgery, but
this would be erroneous. Only those
medical efforts and developments that
could return men to the front or
discharge the disabled back home were
exploited. Moreover, military medicine
in WWI was dependent on scientific
advances largely developed during
times of peace. A careful
review of medical history in general
demonstrates that virtually every
advance in medical science and
practice came to fruition in times not
of conflict, but in times of peace.
Subsequent military medicine has only
built upon the principles established
in the Great War.
War is a ravening beast, appropriating only that which promises its continuation. It will be with us for a very long time. In place of a lasting peace and no further wars, our best hope is for medical science to keep pace with the killing technology practiced by the many in the presence of compassion practiced by the few.
Notes
(1) It
would be another thirty years before the
discovery of penicillin and its use as
the first antibiotic in the waning
months of World War Two.(2) Absolute proof of hemorrhage (excessive bleeding) as the cause of traumatic shock would not come until a decade after the war. (3) The paraffin concept, invented by Col. Andrew Fullerton, was used by A. R. Kimpton and J. H. Brown of Boston to collect donor blood in glass tubes and bottles, transfusing it through rubber tubing and paraffin-coated needles into the recipients (Bird). (4) During WWII, Korea and Vietnam, transfusions with red blood cells alone, plasma or albumin were preferred, but in the recent Gulf Wars, the trend is a return to whole-blood transfusions. (5) The Regimental Medical Officers and litter bearers, being so close to the fighting, sustained high casualty rates. (6) Lung collapse (pneumothorax) was resolved using positive pressure anesthesia through a cuffed tube secured in the trachea (windpipe). (7) The Princess was related to the Radziwills. (8) His nephew, Archibald MacIndoe, also from New Zealand, went on to direct plastic surgery in England during the Second World War, the majority of his patients being pilots shot down and burned during action. (9) Ironically, the grandson of the man who reconstructed shattered faces, Daniel Gillies, is a handsome actor on the TV series The Vampire Diaries.
Works Cited
and Consulted
Bennett, J.D. "Princess Vera Gedroits: military surgeon, poet, and author." BMJ Dec 19 1992; 305(6868): 1532-34. Bird, G.W.G. "The History of Blood Transfusion." Injury: The British Journal of Accident Surgery, Vol. 3, Issue 1 (July 1972): 40-44. Brittain, Vera. Testament of Youth. London: Victor Gollancz, 1933. Cushing, Harvey. From A Surgeon's Journal: 1915-1918. Boston: Little, Brown, and Company, 1936. Delaporte, Sophie. Les médecins dans la Grande Guerre 1914-1918. Paris: Bayard, 1996. Deranian, H.M. Miracle Man of the Western Front: Dr Varaztad H. Kazanjian, Pioneer Plastic Surgeon. Worcester, MA: Chandler House Press, 2007. Dolev, E. "The first recorded aeromedical evacuation in the British Army--the true story." Journal of the Royal Army Medical Corps. Vol. 132, number 1 (February 1986): 34–6. Dunne, J.S, "Notes on Surgical Work in a General Hospital – With Special Reference to the Carrel-Dakin Method of Treatment," British Medical Journal Vol. 1, Number 2984 (Mar. 9, 1918): 283-284. Haber, L.F. The Poisonous Cloud: Gas Warfare in the First World War. Oxford: Clarendon Press, 1986. Hess, J.R. and Schmidt, P.J. "The First Blood Banker: Oswald Hope Robertson." Transfusion 40 (January 2000): 110-113. Larrey, D.J. Memoirs of Military Surgery, and Campaigns of the French Armies. 2 vols. 1814. Birmingham, AL: The Classics of Surgery Library (Gryphon), 1985. Krumbhaar, E. B. "Role of the blood and the bone marrow in certain forms of gas poisoning." JAMA 72 (1919): 39–41. Meikle, Murray. Reconstructing Faces: The Art and Wartime Surgery of Gillies, Pickerill, McIndoe and Mowlem. New Zealand: Otago University Press, 2013. Pelis, Kim. "Taking Credit: The Canadian Army Medical Corps and the British Conversion to Blood Transfusion in WWI." Journal of the History of Medicine and Allied Sciences 56 (2001): 238–77. Preston, Diana. A Higher Form of Killing: Six Weeks in World War I That Forever Changed the Nature of Warfare. New York: Bloomsbury Press, 2015. Santy, P., Moulinier, M., and Marquis, D. "Du Shock Traumatique dans les blessures de Guerre, Analysis d'observations." Bulletin et Mémoires de la Societé de Chirurgie de Paris 44 (1918): 205. Scotland, Thomas, and Hays, Steven, eds. War Surgery 1914-18. West Midlands, England: Helion, 2012. Winter, Jay, ed. The Cambridge History of the First World War. Vol. 1. Cambridge University Press, 2016. "Weapons Effects and War Wounds." United States Army publication. Available at website of Borden Institute, www.cs.amedd.army.mil/borden. Westman, Stephen. Surgeon with the Kaiser's Army. London: William Kimber, 1968. Author's
Biography

Gerald Stulc, MD, FICS
(ret), MFA, Capt. (ret) USNR MC,
completed his residency in general
surgery at Georgetown and a fellowship
in cancer surgery at Roswell Park
Cancer Institute, Buffalo, where he
remained on staff before joining the
clinical faculty at the University of
Louisville.
He was a flight surgeon in the USNR MC for sixteen years, retiring as Captain (2006). After retiring from medicine, he received his MFA in Creative Writing from Spalding University. He has published a number of scientific articles, and recently published a historical novel, The Surgeon's Mate. He is currently working on two nonfiction books, one a history of military medicine from antiquity to the present. His interests are history, collecting antiques and art, scuba diving, and playing the classical guitar. He frequently lectures for the Academy for Lifelong Learning. Dr. Stulc is president of the Saratoga Torch club, and Region One Director. ©2018
by the International Association of
Torch Clubs |